MY BLOG
I AM NOT OK – and that’s OKAY!
By Sharon Orapeleng
13 August 2021
Earlier this week I logged on to my online meeting while working from home and I was immediately immersed within a group conversation about the COVID-19 situation unfolding across Australia. Here at least in Brisbane; we had just come out of a snap lockdown to contain the Delta variant in the community; and were about to return to ‘normality’ – whatever that meant in these Covid times.
The talk about Covid19 has become such a normal conversation starter at meetings and workplaces – replacing the usual mundane weather conversation. It has now become de rigueur to check in about case numbers, restrictions or lock down measures – masks, yes masks and ooh, how we all hate to wear masks etc.
Now as I sat there listening to the ongoing conversation and waiting for an appropriate pause to say ‘Hello, sorry I am late’ (even though it was simply 2 minutes past the scheduled time) I heard ‘Hi Sharon, how are you? – we were just talking about the Covid-19 situation’
I paused and immediately felt as if I was trying to catch my breath, I could feel it escaping me. I knew instinctively I was going to experience a spiral emotional downer. Yes, I was triggered; here in a work meeting with external stakeholders; I was breaking down – tears and all.
You see I woke up that ‘normal’ Brisbane morning like everyone else, but as I checked my phone - a WhatsApp message had come in through the night simply saying ‘Rrangwane Magare is no more’. Five words that shattered my heart. The last few weeks these words announcing that a person I knew was ‘no more’ had become so normal, so expected, so everyday just like the conversation about Covid19 at almost every meeting I attended.
As I began to rumble on about the devastating impact of Covid-19 in my home country Botswana (currently experiencing the highest surge of the delta variant in the world resulting in unimaginable loss of life) I felt that I wanted - I needed - to explain, to tell Botswana’s story, to justify the reason why the tears kept on falling!
I had just been told (yet again) this week, someone I cared about had died; having not long before that, watched (yet another) online funeral of another person I knew who also died of Covid19 complications. This is now over 10 people who I know closely who have passed on in the last three weeks. These are people I grew up with, the people I lived, loved and played with. As I tried to reconcile the obvious contradiction; that here we were living in an environment that was ‘going back to normal’; whilst simultaneously knowing my country of birth was on its knees. Talk around the issue of Covid may be a normal conversation, but these are by no means ‘normal’ times.
These last few weeks my mental, spiritual and physical health has threatened to abandon me – to simply spiral down into some dark abyss so familiar; as I have experienced before, I am now holding on to the smallest thread of hope that still exists and praying it does not completely abandon me.
I am telling you that – I. AM. NOT. OK. I am struggling and I am doing utmost everything in my power to process what is going on around me. The loss. The grief. The anxiety.
A few months ago, I developed a program about Sisterhood Circle focusing on Self-Care to explore the Self- Essentials – Ingredients for Self-Care. This was to be a six-month sisterhood circle journey created to reconnect, restore and re-frame (3 Rs) through monthly zoom sessions and face to face sessions. An educational and self-empowerment group focusing on ingredients for self-care to build protective factors for mental health using culturally focused practices of self-care by tapping into knowledge from ancient cultures as well as innovative practices that have evolved over the years.
Little did I know that this program that I had planned to offer to others was a program that was simply designed for me, to save me. I never knew how much I would tap on to the same strategies that I have developed for others. As I now immerse myself through this Self First program – I am reminded that IT IS OK - NOT TO BE OK. Particularly in these times that we are experiencing which are clearly NOT normal times.
I don’t know how I will react to another death notice. Yes, I expect it - it is just the reality of the times we are living through. Currently I am simply focused on putting a spiritual, physical and mental armoury to give myself the best possible chance of surviving the traumatic and complex grief of Covid19 experiences. It is messy, it is complex – there are many tears, there are moments of no tears and numbness, there are moments of perpetual feelings of jetlag, exhaustion, confusion, self-doubt, zoomies-like energy – the entire gamut of human emotion.
Today on Friday 13 August - I have a day off work as a mental health day where I will be immersing myself into therapy - flotation therapy through my good friends at City Cave Australia as well as few other wellness activities I have planned for today.
Here I am to remind YOU that whatever you are feeling; whatever your ‘NORMAL’ looks like as we navigate our way through this pandemic………… IT IS OK - NOT TO BE OK. Seek help and that is also OK.
If you or someone you know need support-please call the following helplines or visit your local GP .
Lifeline Australia 13 11 14
Suicide Call Back Service 1300 659 467
Kids Helpline 1800 55 1800
MensLine Australia 1300 78 99 78
Multicultural Connect Line 1300 079 020
Coronavirus Mental Wellbeing Support Service 1800 512 348
1300 MH CALL (1300 64 22 55)
Translating and Interpreting Service (TIS National) -131 450
TIS National is for people who do not speak English and for agencies and businesses that need to communicate with their non-English speaking clients
About Self- Essentials – Ingredients for Self -Care
We will relaunch the Sisterhood Circle focusing on Self-Care to explore the Self- Essentials – Ingredients for Self -Care in January 2022.
If you are interested to learn more about our Self-Care and Sistahood Circle please email us at sharon@psychedsolutions.com.au
Hope Beyond Cancer
Hope Beyond Cancer
30 October 2019
By Sharon Orapeleng, Psyched Solutions
October is breast cancer awareness month. This message is coming to you towards the end of the month of October, you may think its perhaps a bit late, however it is never too late to talk about breast cancer and its devastating impact on individuals, families and communities.
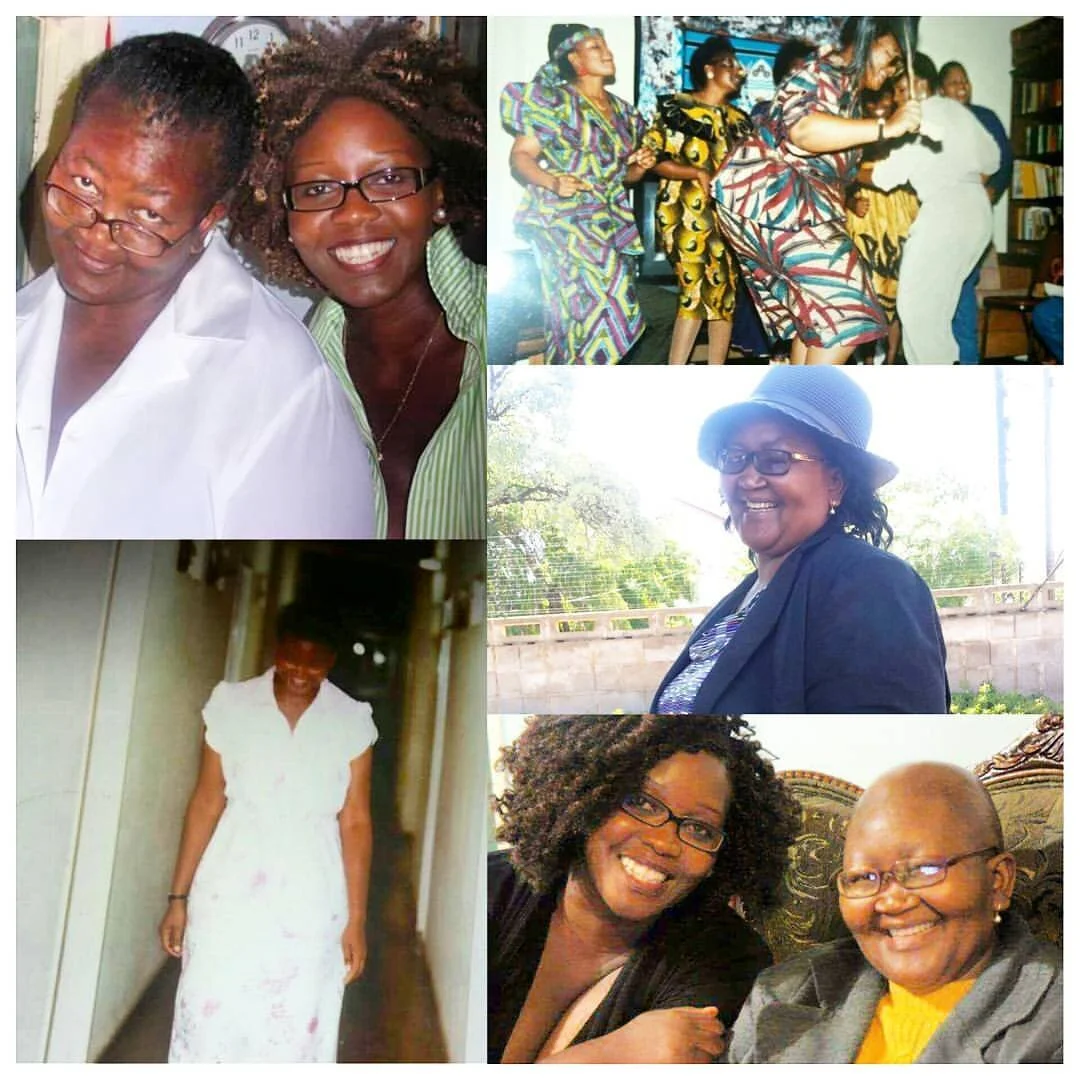
Three months ago I lost my mother Betty from metastatic breast cancer. Although I have experienced loss before – this one was like no other. The death of my mother from a devastating long-term illness has truly shaken the ground I stand on. The pain of loss is indescribable, so as I try to find my footing again, I thought sharing this with you will perhaps help unravel the jumbled thoughts and emotions that persists as I try to adjust to the new normal.
My mother Betty Kegomoditse Sametsi (BKS) Orapeleng was diagnosed with breast cancer in October 2010. The last 9 years she has battled this monster disease which led to her untimely death at the age of 62 in June 2019.
The grieving process began the day mom was diagnosed with cancer, so for 9 years there has been a foreboding sense of anxiety – of potential grief and the loss of her life journey - through this cancer. However, her death has truly and surely amplified this feeling of grief. It is often hard to describe how and what I am feeling as it changes from day to day. As the first-born child of my mother, she became almost an extension of me – I do not know life without her in it.
Recently I went to work wearing mum’s skirt, a beautiful traditional tswana skirt that I found from a pile of her clothes after the funeral. As I walked through the foyer of my work - a colleague stopped me to tell me how beautiful my skirt was – she wanted to know where I bought it, and right there in the middle of the foyer near the lifts I found myself having to say “my mother died, and I have inherited this skirt” . As soon as I said those words I could feel the tsunami of emotional distress coming and there was no stopping it. I rushed to the nearest bathroom, closed the door and curled up in the floor and let the grief take over. I do not know how long I was there for. But I know that when it was over I washed my face, put on my make up and went straight back to my work desk as if nothing happened. No one noticed anything – life went back to normal (or so it seemed).
Navigating grief is as complex as navigating life with the experience of mental illness. The society expect us to be ok - to look ok, but the fact is sometimes I am not OK. And that’s OK. The rug of life has been pulled from underneath me, the emotional comfort I have felt throughout my life with mum is no longer there. Yes I feel vulnerable! Sometimes scared, alone, overwhelmed as I simply do not know how to do life without my mother.
Nothing prepares you to the pain of loss. Having suffered anxiety at times in my life – I know very well the physical manifestation of emotional pain. Grief has been like the anxiety experience - a constant feeling of loss gnawing away which sometimes feels like an experience of a full-blown panic attack.
When does grief becomes too much?
It is important to continue the recognition that grief is a normal response to a human experience with death. We all grieve differently and there is no timeframe for grief. However, over time the intense emotional and physical response of grief should and surely will subside. It may not seem like it sometimes but one day you get to a point when you are able to fondly remember your loved one without the overwhelming feeling of loss and tears associated with the memory.
If in time, the intense feelings of grief do not subside, it may be a sign that things are not going well, and you may need to seek professional help. Like any emotional response to a negative event in your life when it starts to impact of your daily life then there is a problem. Signs and symptoms of concern may look like this:
withdrawal from social and family connections including with family, friends, community etc
disengagements from hobby, work or study
constant feeling of sadness that does not go away,
persistent anger about the loss
sleep disturbances (sleeping too much or not much sleep)
finding no meaning of life
lack of selfcare
alcohol or other drugs dependency
talk of suicide or other suicidal thoughts and behaviours
worsening of a pre-existing mental health issue (anxiety, depression etc)
This extreme form of grieving is called complicated grief or prolonged grief disorder. Most mental health experts agree that six months of unrelenting grief (outside of any pre-existing mental health issue) is enough to cause concern and to encourage professional help. However, this does not mean that you wait for six months before seeking professional help. If any of these signs and symptoms concern you, please encourage professional help at any time.
There are also many things that can assist you create a new normal when death of a loved one has occurred.
My mother BKS often talked about “hope beyond cancer”. She didn’t want cancer nor her experience with the disease to be focal point of our interaction and/or existence. Mum did not survive cancer, but she lived through cancer; she thrived through cancer. Only when she was ready to go, she did.
Her life was truly an inspiration - her life lessons too many to mention. That over 1000 people attended her funeral service was a testament of her life lived, connections made and the touching of countless. She gave us hope and inspiration; that said any stumble in life propels us to greater things. She may only be with me now in spirit and not the physical realm but it is this inspiration that I tap into to help me navigate this new normal.
Few tips that may help you through grieving the loss of a loved one!
Own your feelings
There are days and moments when I do not feel OK and its OK. By noticing how I feel helps me pay attention to my own thoughts and their impact.
Being authentic about your feelings will help you identify strategies to improve your mood and most importantly it will allow others to identify when you need support. Next time if you are not feeling OK – say it? Tell someone how you really feel. You will be amazed about the weight that gets lifted off your shoulders when you ‘own’ your feelings.
Take care of yourself
Grief can feel physically heavy and can take away the joy of living. I have started to prioritise both my physical wellness and mental wellness. I am reconnecting with the things that makes me feel good. Things such as listening to music (yes, I am that girl who blast music in the car), waking up early to watch the sunrise, spending time with my family, walking my dogs etc.
Running a small business, working full time, being mum, wife, community leader/advocate sometimes I find that there is little time for me. Therefore, I make it purposeful to create that time to just be in the moment.
I have also started keeping a gratitude journal, and this helps me focus my thoughts on what I have rather than what I have lost.
Connect to your cultural strengths and/or your religion/spirituality
Within many of the traditional African cultures, life does not end with death, but rather it transitions into a separate realm. Although death itself is unwanted even feared and sometimes seen not a natural occurrence (results of spirits, curse or other demonic interference), when it does occur there is often a belief of the after-life, the existence of a spiritual realm which you connect to if you want to speak with the person who has transitioned.
Many religion and spiritual practices also believe in life after death. This can often bring peace to the bereaved so that although a loved one is not physically here – they are still spiritually here. These practices are seen to be able to shorten the feelings of grief.
Connecting to my cultural strengths and my faith is helping me find meaning beyond this experience of loss.
Celebrating the life that was
Honouring my mother’s legacy is a commitment that I have made to myself. One day I will be able to tell her story, in her own words. Mum kept diaries of words that encouraged her throughout her journey with cancer. Her unwavering faith evident in each of her diary entries. It will be an honour to use these words to inspire others, so I will hopefully one day put it in a book. I have promised her that one day I will write a book about her and it is a promise I will try to fulfil. In the meantime I celebrate my mother by speaking of her, sharing her resilience, living a faithful and resilient life. Her words of encouragements sustaining me and nourishing me.
I will be planting a tree at my house in honour of mum, this is about creating a space of remembrance at my home and nurturing her memory. A tree is a symbol of life and hope.
I will also continue the work of mum in our community in Botswana – revitalising the Semphete Care Centre (in Good Hope, Botswana) which supports the social and emotional wellbeing of vulnerable young kids and out of school youth. In the coming months we will be launching a foundation to help the work and activities of Semphete Care Center.
There are many things that each of us can do to celebrate the life of our dear one who have passed. This helps focus the grief into doing something purposeful and meaningful – something that grief often steals from us.
Love, Live, Smile, laugh
Death of a loved one often robs us from feeling alive again. Connecting with family and friends and allowing yourself to feel their love, their comfort, when they call to say RUOK? When they drag you out of the house so you can do something fun again. Its ok to give yourself permission to love, to live, to smile, and to laugh again.
Yes you will find reasons to smile again. I am beginning to do just that, and it feels good. I know that is what mom would want that, most importantly am doing that for myself!
In 2015 - my mother Betty agreed to guest blog for me about her journey through cancer. You can read her blog here simply titled: The Survival Spirit - I am a Breast Cancer Survivor
Breast cancer is the top cancer in women worldwide and is increasing. In Australia on average, 37 females receive a diagnosis of invasive breast breast cancer everyday. It is important to know more about our breast health for both men and women, understand risk factors and preventative measures, screening and early diagnosis processes, as well as availability and access to appropriate treatment.
Find out more information about breast cancer in Australia here
Hear more from my mother Betty from here
If you or someone you know need support-please call the following helplines or visit your local GP.
Breast Cancer Network Australia 1800 500 258
Breast Screen Queensland 13 20 50
Lifeline Australia 13 11 14
Suicide Call Back Service 1300 659 467
Kids Helpline 1800 55 1800
MensLine Australia 1300 78 99 78
Religion and/or Spirituality on our Mental Health – A Conversation We Must Have!
“I prayed my anxiety away many times” Sharon Orapeleng
It is estimated that almost half (45%) of the Australian population will experience a mental disorder at some time in their lifetime (about 8.7 million people based on the estimated 2017 population). An extract from Our World Data estimates estimates that globally around 970 million people were living with a mental health or substance-use disorder in 2017. There is no denying that mental health issues are one of the biggest challenges in our world today. As a society - as we have more and more public conversations around this issue; and the traditional stigma associated with mental health slowly but surely fades away; it is perhaps likely that we have in fact underestimated just how many of us are impacted in some way by mental health challenges.
Over the last ten years; as well as working in the Queensland mental health system; I have also been proactively raising general community and workplace awareness and understanding of mental health issues through the delivery of several mental health literacy courses including Mental Health First Aid. Lately I have been reflecting on this journey, trying to find the missing link in the narrative. That missing link in the conversation I believe, is the interrelation of religion and/or spirituality with our mental health and how we can harness this resource to positively influence our mental health and emotional wellbeing.
In 2014 after a very traumatic car accident, I was diagnosed with anxiety. As I navigated the system to get help and support for myself, I remember having a conversation with my mother about my diagnosis and she said something to me in Setswana (my mother language); that she often said whenever things were tough; and that is “Modimo o teng” - which is translated in English as “God is there”. This is a phrase my mother used to bring me comfort, meaning and hope to soften any struggles of life.
Religion and/or spirituality is an important source of strength for many people who experience life challenges including mental health issues.
The 2016 Australian Census indicated that Christian religion affiliations were reported by 52% of the population. Non-Christian religions represented about 8% of the population. The 2016 Australian census also recorded that the combined number of people who self-identified as Muslim in Australia, from all forms of Islam, constituted 2.6% of the total Australian population. About 39% of the population stated they had no religion or did not state their religion.
Religion or faith-based affiliation is a significant expression for more than 60% of Australians, therefore a conversation about religion and/or spirituality and its associated outcomes for mental health is overdue. Religion and/or spirituality provides an individual with a sense of connection to something bigger than self and how one fits in with the world. It also creates a sense of community and connectedness, and most importantly gives the individual a sense of purpose and hope. All of these are protective factors for mental health and have positive impacts on the individual’s wellbeing.
Although there are many documented positive impacts of religion and/or spirituality on the overall health and wellbeing of an individual, there is no denying that the religion and/spirituality is expressed differently depending on the individual belief system which is influenced by many factors including cultural factors. This differing belief system can also be detrimental to people’s own health and wellbeing. For example, people who believe that prayer and/or meditation alone will cure their mental health issues are not likely to present voluntarily at a mental health service for care and support. Some individuals would choose different forms of spiritual cleansing such as exorcism over cognitive behaviour therapy and other evidence-based therapies any day.
There is also an increasing stigmatisation of mental health issues in the faith-based communities including the believe that mental illness is caused by lack of prayer and faith or sin; sometimes it is the believe that the evil spirit has influence on the individual experiencing a mental health crisis. This belief system is likely to lead to people being disconnected from communities of support and service providers resulting in a decline in people’s mental health.
Religion and/or spiritual interventions and mental health care and support are not supposed to be mutually exclusive but must interface and align to enable the flourishing of the whole of the person and challenge understanding on perceptions of mental health issues.
My belief is that as long as the mental health sector; and the messaging around mental health and suicide prevention miss this; I fear many people will simply choose to continue to just “pray about it” rather than a combination of prayer or meditation and professional mental health care. Similarly, in cases of individuals faced with severe illnesses such as cancer; this can be observed in evidence of increased mortality where individuals embrace alternative therapies at the exclusion of conventional medicine when often the best outcomes are seen by those who incorporate both in combination.
There is no doubt that religion and/or spirituality forms a part of the individual’s core understanding of the world they live in and how they interact with it and others. Most poignant on this is the application of religion and or/spirituality as a coping mechanism for people from ethnic communities which bring enormous implications in relation to explanatory models of mental health issues, service access and treatment.
If you were to ask me about the impact of my faith in my recovery journey from anxiety – I will tell you that “I was spurred on by my mother’s favourite phrase of ‘Modimo o teng’ – and yes I prayed my anxiety away many times, but I also saw my doctor, had a mental health care plan, took medication, saw a psychologist and did many other things to keep me well and still do”
Mental Health is such a challenging issue, we must identify and utilise every possible tool at our disposal in a collaborative sense so that no one is left behind, no one feels isolated and no one ever feels the need to choose faith and/or spirituality over professional mental health care and support. As unlikely bedfellows as it seems, they are not meant to be mutually exclusive.
Upcoming Community Conversations
If you are interested to be part of discussions on this topic – Sharon Orapeleng will be hosting a series of community conversations on Religion and/or Spirituality and Mental Health in Brisbane from September 2019. If you are interested to know more details please send email to sharon@psychedsolutions.com.au or check the website on www.psychedsolutions.com.au for further updates.
Follow Sharon Orapeleng on social media Twitter- @sharonora Facebook - @SharonOrapeleng Linkedin @SharonOrapeleng
If this topic has caused any concerns for you or someone you know, please call the following helplines or visit your local GP.
Lifeline Australia 13 11 14
Suicide Call Back Service 1300 659 467
Kids Helpline 1800 55 1800
MensLine Australia 1300 78 99 78
Looking for support and advice, call beyond blue - 1300 22 4636
Australian Migration Debate- Changing the African Narrative
In August, Queenslanders have a month of celebrating our cultural diversity. This is the State’s largest celebration of multiculturalism which acknowledges that regardless of our different journeys to these shores, in Queensland we are welcomed.
This is the time where everything “exotic” is celebrated. Many people have the opportunity to try something new, whether it is the food, music and dancing, or perhaps watch a multicultural fashion show. This is celebration of us in all our diversity.
However, as an African Australian, I cannot help but feel a sense of uneasiness as I continue to watch the unfolding story in the media and the political spotlight that continues to dehumanise a section of our community.
The headlines and discerning voices are amplified and continue to vibrate throughout my consciousness – “…. they don’t belong, they don’t integrate, send them back to where they come from, they are responsible for crime, they are gangs, people are afraid to go out at night because of them….” A continuous narrative aimed at marginalising African Australians mainly in Victoria, but spreading rapidly across the whole nation.
This current narrative about African Australians is insidious, it damages the whole of our celebrated multiculturalism. This narrative threatens to exclude African Australians from the basic human equality, their belonging to this greatest southern land of Australia in question, their voices muffled and silenced.
This continuous spotlight on our communities devalues our stand in the wider Australian community and the most disheartening thing is that it is spearheaded by political propaganda and mistruths.
The collective bashing of our communities’ identity leads to our model multicultural Australia being accustomed to performing and entrenching racism, discrimination and oppression of African Australians. This rhetoric is simply wrong and must be condemned.
More importantly the consequences of words being spat around so carelessly impact deeply on our young people. It further marginalises them, it throws questions about who they are, their worth, their contribution, their belonging.
It is surely our duty as Queenslanders, and Australians to stand together and condemn the apparent deployment of dehumanising language which only leads to societal hierarchy, social isolation, mental health issues and can certainly lead to targeted hostility and violence directed towards African Australians.
We cannot sit back and allow racism to manifest, we must demand better from our nations leadership, we must expect responsible media reporting including a media code of practice that abates explicit focus on ethnicity and race when reporting crime.
It seems like we have learned nothing from the past; that the singling out of a community relating to actual or perceived criminality; has everlasting impact on their well-being and integration. The continual marginalisation of each new wave of ethnic minorities - whether they Italian, Greek, Vietnamese, Lebanese & other Muslim countries, Chinese and now of course African nations – is historically driven by a small but increasingly vocal and agitating minority. When the vast majority of Australians have positive experiences with each new wave – so much so that inevitably the food and culture of each ‘New Australian’ becomes part of our national psyche, our national identity – why therefore do the media pander to the disruptive narrative of a few closed minded groups that assume they speak on behalf of us all, when nothing could be further from the truth.
Surely there comes a time when there is a realisation that we simply cannot continue to travel this road again and again. Racism should and cannot be an acceptable part of our identity as a nation. We cannot let the vocal minority of racist right wing section of our community threaten our racial and social harmony.
This August, during multicultural month, let me remind Queenslanders that we need to redouble our efforts and commitment to end racism in all sections of our community and it starts with you and me! Our diversity is our strength and we must work hard to keep it that way!
Author: Sharon Orapeleng is a community advocate, a mental health professional and Principal Consultant at Psyched Solutions.
Lets have a conversation about saving lives!
I was recently speaking to a friend about issues around mental health, and the impact to the individual, families and communities. Somehow the conversation drifted to the topic of suicide and suicidal thoughts and behaviours.
My friend said to me “I truly believe that people who take their own lives are so selfish, there is no problem in the world that equates to ending your life”. As I sat there listening to this friend narrate the story of people she knows who have taken their own life, who she perceives as “ungrateful” and “going to hell” – passing judgement - I could feel the urge to immediately stop the conversation as it was becoming too “uncomfortable”.
I kept asking myself questions - How can I change the perception of people like her who believe suicide and suicidal thoughts and behaviours are an abomination? That suicide is simply unforgivable?
Unfortunately, her perception of suicide is very common. There is already existing stigma around people who occasionally struggle with everyday life due to various mental health issues and other social factors. There are good days and bad days, but some days are much, much worse.
When it comes to suicidality many people suffer in silence because of the “shame” of admitting to themselves and others around them that they feel like “life is not worth living”. That they may get called “selfish” “uncaring” and all other names. They carry the guilt of feeling how they feel, increasingly feeling isolated from the “accepted community judgement and perceptions”.
People who think about suicide are in pain, a silent pain that feels like a bottomless pit, it has no end and can be all too consuming and debilitating. To them it is not necessarily wanting to end their own life, it is more about wanting the pain they feel to stop.
This is how I explained it to my friend during our long conversation, and when she said to me “But how do you know this? How do you know it is emotional pain they feel?” I said to her “It is because I have known that pain”. She looked at me with almost unbelieving eyes – “but you are one of the strongest people I know, how, why…..”. She had no more words at that moment.
You see, there is no such thing as a “typical” sufferer, and those who do feel these thoughts are often very adept at hiding it even from their closest friends and colleagues – which is why it can come across as a seismic shock when someone within our circle of contacts succumbs to their internal demons.
I am grateful for the conversation like the one I had with my friend and; over the course of years, many others; because conversations such as this can help remove the stigma associated with mental health issues and suicidal thoughts and behaviours. Conversations such as this can change perception and conversations like this can help build understanding and compassion.
Conversations like this can help save a life.
How can we stem the tide of this preventable death by suicide if we are unable to talk about it? As for me, this is a conversation that must be heard!
Here are some facts about this suicide we should all be aware of:
According to Australian Bureau of Statisticsdata on suicide deaths in Australia, over 3,000 people died by suicide in 2015. That equates to around 8 people who tragically take their own live in Australia every single day.
Over 65,000 Australians make a suicide attempt every year
Around 400,000 Australians experience suicidal thoughts every year
Around 35,000 Australians are admitted to hospital for suicide-related injuries every year
Suicide is the leading cause of death for Australians between 15 and 44 years of age.
Many people who die by suicide have experienced a mental illness.
Often people who are considering suicide are dealing with a combination of poor mental health and difficult life events.
Individual and community’s perception of suicidal behaviour can play an important role in preventing suicide or the degree to which suicidal behaviour is disguised. The great majority of people who experience a mental illness do not die by suicide. However, of those who die from suicide, more than 90 percent have a diagnosable mental disorder. It is critical that we must learn how to have the conversation about suicide and how to safely support someone thinking about suicide.
To tie in with the National R U OK Day on Thursday September 14 - which inspires and empowers everyone to meaningfully connect with people around them and to support anyone struggling with life by starting the conversation around mental health – I am hosting “The MHFA for Suicidal Person”. This will provide you with practical skills and knowledge about how to safely support when someone is experiencing suicidal thoughts and behaviours and allows you to practice these skills in a safe environment.
You will learn:
· Understanding accurate information about suicide in the Australian context.
· How to identify signs and risk of suicide
· First aid guidelines of how to help when someone is experiencing suicidal thoughts and behaviours
· Practicing these skills in a safe environment.
MHFA for the Suicidal Person Course is not a postvention course and is not recommended for individuals recently bereaved by suicide. The MHFA for the Suicidal Person Course is not a therapy course but will help you to learn more about suicide prevention and how to have the conversation that can save a life as well as where to get help and support.
Course Format:
This is a 4-hour face to face course to be held on Thursday 14 September 2017 from 1pm to 5pm.
Please Note: We run this course in small group numbers which allows creation of a safe and comfortable space for participants and allows us to provide support and care needed. Reserve your space now.
Pricing: $99 (incl. GST) per person
Course participants receive a Handbook to keep and receive a digital Certificate of Completion when you submit online feedback.
Places are limited. For registration or more information, please contact us on 0411 330 382 or send us email to sharon@psychedsolutions.com.au
Completion of this course does not accredit you to become Mental Health First Aider - you need to complete the 12 HR Standard Mental Health First Aid Course if you want to be accredited as a Mental Health First Aider.
If interested in the accredited 12 Hr Mental Health First Aid Course – our upcoming public course is on Friday 10 November 2017 and Saturday 11 November 2017. Spaces are limited so please reserve your booking here.
Lending a helping hand during mental health distress through Mental Health First Aid
Mental health pain is as real as any physical pain to any part of the body. However, unlike physical pain where sometimes the injury is visible or physically and behaviourally expressed, mental health pain can be a very hidden, isolating, deep dark pain that may seem to have no end. Whether it is physical pain or mental health pain both require some sort of intervention to ease the pain or stop the pain and without intervention it can lead to a crisis situation. The importance of knowing what to do, how to do it, when to do it, and who to call for support can be a matter of life and death.
Mental health issues are more common than you think. One in five of us will experience a common mental health illness such as depression, anxiety or alcohol and other drug misuse in each year. This means someone in your close friend circle, work mate, family, community, or even yourself may suffer the impact of mental health illness at some point in your life.
Just like physical first aid and CPR, mental health first aid is a life skill, the course teaches you to identify the early signs of developing mental health issues and to know of local mental health services and support systems available as well as ability to respond effectively during a mental health crisis situation; such as someone experiencing suicidal thoughts and behaviours; until professional help is accessed.
For Sharon Orapeleng, a mental health professional and Director of Psyched Solutions with accreditation to deliver the mental health first aid course, this issue is personal. “
“Mental health issues are the reality of many Australians every day and helping to create awareness around the impact of these issues is something I am very passionate about, because it can save a life” she said.
Diagnosed with Post Traumatic Stress Disorder and anxiety a few years ago Sharon knows first-hand the debilitating impact of mental illness and how early intervention can help save a life.
“As a mental health professional working in the mental health system, and wearing many hats as a mother, wife, community leader, advocate and consultant; I was the one who always helped anyone who needed help, always doing for others; and when a car accident turned my life around, no one outside my immediate family noticed I was struggling, no-one noticed I needed help” She said.
“It was easier to talk about the physical pain, the back surgery, the struggle to walk, the physical healing but the emotional pain remained and until I received the help needed.”
“You never know what is around the corner, your life can change in a second and knowing what to do, how to help yourself or lend a helping hand to another person during the struggle with mental health issues is critical.”
Sharon has been delivering mental health first aid course for over five years to the public, government and non-government organisations such as Australian Red Cross and many others. In 2016 she teamed up with Brisbane rugby community through the newly formed organisation “Rugby Unite” to raise mental awareness in the community of rugby as their Mental Health First Aid Course Instructor.
“The aim of the Rugby Unite organisation in partnership with Mental Awareness Foundation is to have every rugby club in Queensland to have a trained Metal Health First Aid Officer including players, coaches, referees and club members, to create a supportive community that allows for mental health issues to be talked about and help people access much needed help” Sharon said.
To register for Sharon’s upcoming accredited Mental Health First Aid Course on Friday 30 June and Saturday 1 July 2017 in Ashgrove, Brisbane contact Sharon at Psyched Solutions, www.psychedsolutions.com.au or call 0411 330 382. Direct link for booking is here
To learn more about Mental Health First Aid go to www.mhfa.com.au
Mental Health First Aid for the Suicidal Person - A new short Course!
The international theme for World Mental Health Day in 2016 is: Dignity in Mental Health - Psychological & Mental Health First Aid for All: http://wfmh.com/world-mental-health-day/
To tie in with the World Mental Health Day, Mental Health First Aid launched a new course 'MHFA for the Suicidal Person' a half day (4hrs) stand alone face-to-face MHFA course which teaches participants how to apply suicide first aid skills to save a life.
The Australian Bureau of Statistics recently released data on suicide deaths in Australia. In 2015, over 3,000 people died by suicide, that equates to around 8 people who tragically take their own live in Australia every single day.
These statistics on suicide are incredibly sobering and highlights the need to break down stigma attached to this taboo subject. Suicide and thoughts of suicide is a reality for many people every single day.
We are pleased to be able to offer this short course on 'MHFA for the Suicidal Person' which allows us to focus the attention on this topic and teach people how to provide first aid skills to anyone with suicidal thoughts and behaviors and support the person to access professional help.
Having a conversation about Suicide breaks down the stigma and saves life!
Contact us to arrange for the 4hrs - MHFA for the Suicidal Person course for your organisation or community.
If this topic has caused any concerns for you or someone you know, please call the following helplines
Lifeline Australia 13 11 14
Suicide Call Back Service 1300 659 467
Kids Helpline 1800 55 1800
MensLine Australia 1300 78 99 78
Looking for support and advice, call beyond blue - 1300 22 4636
Translating and Interpreting Service (TIS National) - 131 450
Have a great Mental Health Week!
Sharon Orapeleng, Director and Trainer
Psyched Solutions
Suicide: Dispelling the Myths and Changing the Conversation!
Warning: This blog contains material about suicide which may be triggering to some readers.
“Suicide” is one of the last remaining taboo topics in an age when nothing no longer seem off limits. Not many want to openly talk about it ‘just in case it may put thoughts of suicide in people’s mind’ they may say. However the reality is that suicide touches the lives of many people and has devastating impact on family, friends, colleagues and community. Many people take their own lives every day in Australia and around the world. In 2013, about 6 people died by suicide every day around Australia, that is around 2,500 people who took their own lives. Approximately 75% of those who died by suicide were males and 25% females in 2013. Women are however 4 times more likely to attempt suicide with hospital data for the 2008-2009 financial year indicating that 62% of those who were hospitalised due to self-harm were women.
These statistics are incredibly sobering and highlights the need to break down stigma attached to this taboo subject. Suicide and suicidal ideation is a reality for many people every single day. Just recently on social media (Facebook) I have been witnessing a number of viral posts about suicide, one of them that struck the cord with me is this one below;
“Many people think that a suicide attempt is a selfish move because the person just does not care about the people left behind. I can tell you that when a person gets to that point, they truly believe that their loved ones will be much better off with them gone. This is mental illness not selfishness. TRUTH: Depression is a terrible disease and seems relentless. A lot of us have been close to that edge, or dealt with family members in a crisis, and some have lost friends and loved ones. Let's look out for each other and stop sweeping mental illness under the rug. If I don't see your name, I'll understand. May I ask my family and friends wherever you might be, to kindly copy and paste this status for one hour to give a moment of support to all those who have family problems, health struggles, job issues, worries of any kind and just need to know that someone cares. Do it for all of us, for nobody is immune. Hope to see this on the walls of all my family and friends just for moral support. I know some will!!! I did it for a friend and you can too. You have to copy and paste this one, no sharing. Thank you” (Author Unknown)
I have seen many friends sharing this above statement on their walls. This highlights the power of social media in breaking down the walls on these sensitive topics such as suicide and mental illness. A very welcomed change! However there are still a number of myths associated with suicide and the discussion around it can quickly get hijacked by those who are misinformed about the topic which can have devastating impact on those bereaved by suicide. The viral post above touches on one of the most common myths associated with suicide which labels victim of suicide as “selfish, not caring etc.” This labeling of the person who has died by suicide as selfish or not caring fails to take to account the fact that research has consistently shown a strong link between suicide and depression, with 90% of the people who die by suicide having an existing mental illness or substance abuse problem at the time of their death.
There are many more myths about suicide, here are some of the most common:
Myth: People who talk about suicide don’t actually do it
Fact: Many people who complete the act of suicide spend considerable time prior to the act, talking about it
Myth: Asking a person who is suicidal whether they are thinking of taking their own life will make them do it
Fact: By giving the person who is suicidal permission to discuss their feelings, is often the best opportunity to make them aware that somebody cares about their life and give them hope for life.
Myth: Only certain types of people commit suicide
Fact: Suicidal thoughts and actions can affect anyone from any socio-economic group, religious or racial background or age
Myth: Suicidal people want to die
Fact: People who are suicidal just want to end the intense emotional and/or physical pain they are experiencing
This clearly highlights the need for more public awareness about suicide. We need to have the capacity to identify signs of symptoms of a developing mental health issue such as depression and be able to respond to a crisis situation such as someone thinking of suicide. How do you appropriately provide support needed for someone who finds the courage to tell you that they are thinking of taking their own life? How do you give someone hope for life who life has ran them into a rut and they see taking their own lives as the only way to make the hurt stop? How do you support those who are left bereaved by suicide?
Suicide is a permanent solution to a temporary problem. It is important to talk about it so we can understand how to prevent it.
Join us at our next Mental Health First Training on the 6th – 7th November, 2015 in Brisbane as we discuss about what you can do to support someone in a crisis situation such as having suicidal thoughts and behaviours as well as understand the signs and symptoms of common mental health issues and what you can do to help. Help us break the stigma associated with mental health illness so we are able to help ourselves, families, colleagues and community.
This could be one of the most important decisions you may ever undertake, to learn an important life skill that will not only help you, but more importantly someone in need close to you.
Book here
I look forward to seeing you at the training!
If this topic has caused any concerns for you or someone you know, please call the following helplines
Lifeline Australia 13 11 14
Suicide Call Back Service 1300 659 467
Kids Helpline 1800 55 1800
MensLine Australia 1300 78 99 78
Looking for support and advice, call beyond blue - 1300 22 4636
Translating and Interpreting Service (TIS National) - 131 450
Changing Perceptions and Removing the Stigma about Mental Illness
Mental health issues are among the leading causes of disability across the globe. Many people do not associate mental illness with disability however moderate to severe mental health issues can be as disabling as physical disability. Mental health issues do not discriminate, anyone can develop mental illness at some point in their lives. In Australia 1 in 5 people will be diagnosed with a common mental health issue in any given year. The risk factors are wide and varied. The stigma associated with mental illness and the negative and discriminatory attitudes can have devastating impact on the person struggling with the illness. Community awareness about mental health issues is very important to help change perceptions and remove the stigma.
This week (04-10 October, 2015) is the National Mental Health Week held to coincide with World Mental Health Day on 10 October, 2015. These national events are an opportunity to create awareness around mental health and well being and equip people with the right information.
Connect with you local mental health organisations to participate in a number of events planned for this week.
Media is important in changing perceptions and removing stigma about mental illness. Watch out for ABC TV and radio's Mental As programs during this national mental health week. From comedy, to documentaries, Q and A, and entertainment, ABC is leading to challenge the stigma associated with mental illness and start the conversation. Find out more here.
Mental Health Australia is running a campaign aimed at acknowledging your role in looking after your own mental health and well being. The 'Mental Health Begins With Me' campaign is about making a mental health promise to yourself then sharing it with your family, friends and colleagues. Visit campaign website here to make your mental health promise.
Lets join together and change perceptions around mental health issues and urge services to appropriately and effectively support people with mental health issues.
If you live in Australia and are you need someone to talk to - call one of the following numbers:
Lifeline - 131 114 beyondblue - 1300 22 4636 Kids Helpline - 1800 55 1800
Suicide Call Back Service -1300 659 467
Translating and Interpretation Service (TIS National) - 131 450